Tissue Viability – Prevention and management of pressure ulcers/injuries
What is a pressure ulcer?
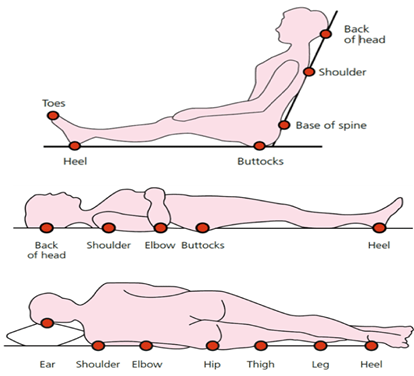
Pressure ulcers, also known as pressure sores or bedsores, are areas of skin and tissue that get damaged when you stay in one position for too long. This can happen if you’re sitting or lying down and unable to move easily.
When the same part of your body is under pressure for a long time, it can stop blood from flowing properly to that area. Without enough blood, the skin and tissue don’t get the oxygen and nutrients they need, which can lead to damage. Without proper care, pressure ulcers can get worse. They can be painful and may damage not just the skin, but also the muscles and bones underneath.
More information can be found on the NHS UK website – Pressure ulcers (pressure sores) – NHS.
Risk, prevention, management and support
Further information and resources
Safeguarding
If you believe that an individual may be a victim of neglect, abuse or cruelty, you can report a safeguarding concern at Report a safeguarding concern – Safeguarding reporting for the public – Lincolnshire County Council. You do not need to know everything about the situation. You may just be worried or feel that something is not right.
Our work | Our campaigns | ‘Let’s talk’ health and wellbeing Lincolnshire | News